Table of Contents
Togglegut-brain axis: how the microbiome influences anxiety and depression.
The Gut-Brain Axis: A Complex Relationship
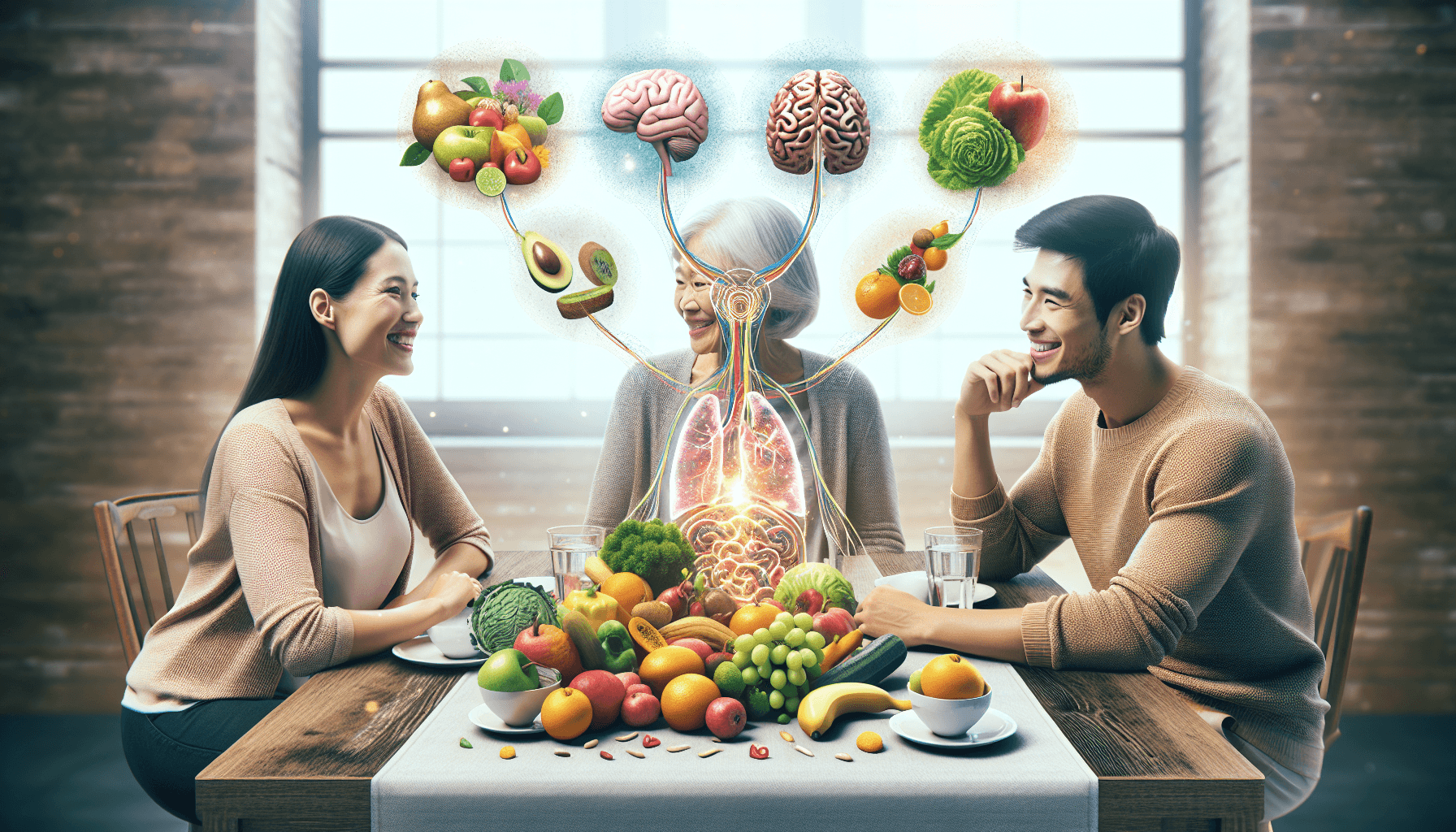
The gut-brain axis represents a vital communication network between the gastrointestinal tract and the central nervous system (CNS). This connection is shaped by the microbiome, which consists of trillions of microorganisms residing in the intestines.
Key points to consider:
- The gut microbiome significantly influences mental health, affecting mood and behavior.
- Disturbances in gut bacteria can lead to conditions such as anxiety and depression.
- Various mechanisms, including neurotransmitter production and immune system regulation, illustrate how gut health impacts mental wellness.
Understanding this complex relationship emphasizes the importance of maintaining a balanced microbiome for optimal mental health outcomes.
Understanding the Gut-Brain Connection
The gut-brain axis is a complex network defined by bidirectional communication between the gastrointestinal tract and the central nervous system (CNS). This relationship allows for constant interaction, where signals from the gut can influence brain function and vice versa.
Gut-Brain Axis
Key Components of Communication:
- Neural Pathways: The vagus nerve serves as a major conduit for signals traveling between the gut and brain.
- Hormones and Neurotransmitters: Gut bacteria produce various neurotransmitters, such as serotonin, which play vital roles in mood regulation.
- Immune Signaling: The gut microbiome interacts with the immune system, producing metabolites that can influence inflammatory responses affecting mental health.
Importance for Health:
The significance of this connection extends to various aspects of health, particularly mental well-being. Disruptions in gut health can lead to altered brain signaling, potentially contributing to disorders like anxiety and depression. A balanced gut microbiome supports not just digestive health but also emotional stability, illustrating the profound impact of gut health on your overall mental state. Understanding this connection opens avenues for innovative approaches to enhance mental wellness through dietary and lifestyle modifications.
Also Read.
The Surprising Link Between Parkinson’s Disease and Vitamin B Deficiencies
The Role of Gut Microbes in Mental Health Disorders
1. Neurotransmitter Production: The Gut’s Influence on Mood Regulation
The gut microbiome, which consists of trillions of microorganisms, plays a crucial role in the production and regulation of neurotransmitters that are essential for mood regulation. One of the most important neurotransmitters is serotonin, with approximately 90% being produced in the gastrointestinal tract. This highlights the significant connection between gut health and emotional well-being.
Importance of Serotonin
- Mood Regulation: Serotonin is often referred to as the “feel-good” neurotransmitter because it contributes to feelings of happiness and well-being.
- Impact on Anxiety and Depression: Low levels of serotonin have been linked to increased susceptibility to anxiety and depression. Individuals with these mental health disorders often exhibit altered serotonin pathways.
Role of Gut Bacteria in Synthesizing Neurotransmitters
The gut microbiota influences the production of various neurotransmitters, including:
- Serotonin: Specific strains of gut bacteria are involved in converting dietary tryptophan into serotonin. This process highlights how dietary choices impact mood regulation through microbial activity.
- Gamma-Aminobutyric Acid (GABA): Another important neurotransmitter that helps regulate neuronal excitability throughout the nervous system. Certain gut bacteria can produce GABA, thus promoting relaxation and reducing anxiety.
These microorganisms create a complex network that involves multiple biochemical pathways influencing neural signaling. When gut bacteria thrive, they enhance neurotransmitter production, contributing positively to mental health.
Gut-Brain Axis
Impact of Altered Neurotransmitter Levels on Mental Health Conditions
Disturbances within the gut microbiome can lead to dysregulated levels of neurotransmitters. Factors contributing to this imbalance include:
- Dysbiosis: An imbalance in gut microbial populations can disrupt normal neurotransmitter synthesis. For instance, antibiotic use can deplete beneficial bacteria that synthesize serotonin.
- Dietary Choices: Poor nutrition lacking in prebiotics and fiber can adversely affect microbial diversity and overall function.
Research indicates that individuals experiencing mental health issues such as anxiety and depression often show distinct differences in their gut microbiota compared to those without such conditions. These differences may manifest not only psychologically but also physiologically, with gastrointestinal symptoms accompanying psychological distress.
Recognizing the role of the gut microbiome in mental health opens avenues for therapeutic approaches targeting these microorganisms. Interventions focusing on restoring microbial balance could potentially improve neurotransmitter production and mitigate symptoms related to mood disorders.
This intricate relationship between gut microbes and mental health emphasizes the necessity for maintaining a healthy microbiome through lifestyle choices, particularly diet. Understanding these interactions lays a foundation for future exploration into effective treatments that harness the power of our gut flora for better mental health outcomes.
High-Fat Diets and Anxiety: Mechanisms and Management
2. Dysbiosis: When the Microbiome Goes Awry
Dysbiosis refers to an imbalance in the gut microbiome, which consists of a diverse array of microorganisms that play essential roles in maintaining physiological functions, including mood regulation and behavior. Several factors can contribute to dysbiosis, including:
- Antibiotic Use: These medications can disrupt the natural microbial balance, leading to reduced diversity.
- Poor Diet: Diets high in processed foods and low in fiber can negatively affect the composition of gut bacteria.
The relationship between dysbiosis and mental health disorders is significant. Research indicates that alterations in the gut microbiome can lead to increased levels of inflammation and changes in neurotransmitter production, such as serotonin, which directly impact neural signaling. Specific findings include:
- Anxiety: Dysbiosis has been associated with heightened anxiety-like behaviors in both animal models and humans.
- Depression: Individuals experiencing depression often exhibit distinct microbiome profiles compared to healthy counterparts, indicating a strong link between microbial health and mood.
Understanding dysbiosis emphasizes the importance of a balanced gut microbiome for mental well-being. Addressing these imbalances may offer promising avenues for alleviating symptoms associated with anxiety and depression.
The Bidirectional Relationship Between Stress and Gut Microbiota
Chronic stress can significantly disrupt the balance of gut microbes, leading to a condition known as dysbiosis.
1. How Stress Affects the Gut
- Stress Response: When you experience stress, your body’s response activates the hypothalamic-pituitary-adrenal (HPA) axis, which can alter gut permeability and microbial composition.
- Microbial Composition Changes: Research shows that stress-induced changes may favor pathogenic bacteria over beneficial strains, impacting gut health.
10 Superfoods For Better Immunity
2. How Gut Health Affects Mental Health
The implications of these changes extend beyond physical health. Altered microbial composition can influence behavior and mood disorders in several ways:
- Behavioral Changes: Studies indicate that individuals experiencing chronic stress often display anxiety-like behaviors linked to shifts in gut microbiota.
- Mood Disorders: The imbalance may exacerbate symptoms of depression, contributing to a cycle where poor mental health further affects gut health.
This intricate relationship emphasizes the importance of managing stress not only for mental well-being but also for maintaining a healthy gut microbiome. Understanding this dynamic can guide therapeutic approaches targeting both mental health and gut health for more effective treatment strategies.
Exploring Therapeutic Approaches Targeting the Gut-Brain Axis for Mental Health Treatment
1. Dietary Modifications: Nurturing Your Gut for Better Mental Health
A balanced diet plays a pivotal role in maintaining a healthy gut microbiome, which can significantly influence mental health. Specific dietary interventions can help cultivate beneficial gut bacteria, ultimately supporting mood regulation and reducing the risk of anxiety and depression.
Importance of a Balanced Diet
To nurture your gut microbiome, focus on incorporating the following elements into your daily meals:
- Fiber-Rich Foods: Foods high in fiber, such as whole grains, fruits, and vegetables, serve as fuel for beneficial gut bacteria. This promotes a diverse microbial community that is crucial for optimal gut health.
- Fermented Foods: Incorporating fermented foods like yogurt, kefir, sauerkraut, kimchi, and kombucha can introduce live probiotics into your diet. These foods help replenish and maintain a healthy balance of gut microbes.
- Prebiotics: Prebiotic foods such as garlic, onions, asparagus, and bananas contain compounds that stimulate the growth of beneficial bacteria. Including these in your diet can enhance the overall health of your gut microbiome.
Practical Tips for Incorporating Gut-Friendly Foods
Making dietary modifications may seem challenging at first. Here are some practical tips to integrate gut-friendly foods seamlessly into your routine:
- Start with Breakfast: Opt for a bowl of oatmeal topped with fruits and seeds or enjoy a smoothie made with yogurt and spinach to kickstart your day.
- Snack Smartly: Replace processed snacks with options like nuts, seeds, or hummus with veggies. These choices provide both nutrients and fiber.
- Experiment with Fermentation: Try making homemade sauerkraut or pickles to add to meals. These not only enhance flavor but also boost probiotic intake.
- Explore New Recipes: Incorporate recipes that highlight prebiotic and probiotic ingredients. For example, consider dishes featuring garlic-roasted vegetables or miso soup.
- Stay Hydrated: Adequate hydration supports digestion and helps maintain a healthy microbiome. Aim to drink plenty of water throughout the day.
- Gradual Changes: Transitioning to a gut-friendly diet doesn’t have to happen overnight. Gradually introduce new foods while phasing out less nutritious options to create lasting habits.
Integrating these dietary modifications fosters an environment conducive to gut health and mental well-being. Focusing on whole foods rich in fiber, fermented products packed with probiotics, and prebiotic-rich ingredients can create significant positive shifts in emotional health over time. By prioritizing what you eat, you empower yourself to take charge of both your physical health and mental wellness on this journey toward better overall well-being.
2. Fecal Microbiota Transplantation (FMT): A Promising Frontier in Mental Health Research
Fecal microbiota transplantation (FMT) involves transferring fecal matter from a healthy donor to a recipient, with the goal of restoring a balanced gut microbiome. This procedure has gained attention for its potential applications in treating mental health disorders.
Process of FMT:
- The donor’s stool is screened for pathogens.
- After processing, the fecal matter is introduced into the recipient’s gastrointestinal tract through various methods, such as colonoscopy or oral capsules.
Potential Benefits:
- FMT may help individuals suffering from anxiety and depression by reestablishing a healthy microbial community.
- Alterations in gut microbiota composition have been linked to mood disorders, making FMT an intriguing therapeutic strategy.
Current research indicates promising results regarding FMT’s effectiveness:
- Clinical studies suggest that patients receiving FMT experience improvements in mood symptoms.
- Evidence supports specific probiotic strains’ efficacy for enhancing mental well-being, highlighting the importance of modulating the gut microbiome.
While more studies are needed to solidify these findings, FMT represents an innovative approach in addressing mental health conditions through gut health restoration.